Common information
A complete of 59,231 sufferers with gastric most cancers had been enrolled on this examine, together with 35,889 (60.6%) males and 23,342 (39%) females. 70.9% of sufferers (n = 41,995) had been Caucasians, 13.1% (n = 7776) had been African American and 16% (9460) from different ethnicities. Metastasis to the mind was reported in 368 (0.62%) sufferers.
Traits of sufferers with or with out metastasis
It was discovered that mind metastasis was considerably extra widespread in sufferers aged youthful than 60 years, males, Caucasians, sufferers with major tumor web site of the cardia, grade IV, unknown T stage, unknown N stage, sufferers with no earlier surgical procedure for major tumor and in whom most cancers had metastasized to different organs equivalent to bone, liver and lung (P < 0.05). There was no important affiliation between revenue and histological kind of tumor and mind metastasis (Desk 1).
Univariable and multivariable logistic regression evaluation of odds of gastric most cancers mind metastasis
Univariable evaluation outcomes steered that tumor web site in abdomen, race, age, gender, T stage, N stage, tumor grade, metastasis to bone, liver and lung, surgical procedure of major tumor, tumor dimension and histological kind had been important impartial threat components for mind metastasis (P < 0.05), whereas revenue was not a big threat issue for mind metastasis (P > 0.05) (Desk 2).
All important components from the univariable evaluation had been entered in to the multivariable logistic regression mannequin. Danger of mind metastasis was considerably decrease in sufferers older than 60 years, in comparison with sufferers youthful than 60 years (adjusted odds ratio [aOR] 0.680, 95% CI 0.547–0.846). Males had been at a considerably increased threat of mind metastasis in comparison with females (aOR 1.294, 95% CI 1.017–1.647). Danger of mind metastasis was considerably higher in sufferers who had developed metastasis to lung (aOR 3.943, 95% CI 3.101–5.013) and bone (aOR 3.845, 95% CI 3.020–4.896). Sufferers with Grade II most cancers (aOR 4.387, 95% CI 1.367–14.081), Grade III most cancers (aOR 3.819, 95% CI 1.204–12.109), Grade IV most cancers (aOR 7.961, 95% CI 2.049–30.921) and sufferers with unknown grade (aOR 5.420, 95% CI 1.704–17.238) had been extra prone to develop metastasis to mind as in comparison with sufferers with Grade I tumors. Sufferers who underwent surgical procedure of major tumor had been at considerably decrease threat of mind metastasis (aOR 0.210, 95% CI 0.131–0.337). Danger of mind metastasis was lesser in sufferers with major tumor of antrum (aOR 0.267, 95% CI 0.158–0.452) and physique (aOR 0.530, 95% CI 0.340–0.827), in comparison with cardia. Sufferers at N3 stage (aOR 2.527, 95% CI 1.548–4.127) and sufferers with unknown N stage (aOR 1.459, 95% CI 1.110–1.917) had been at higher threat of mind metastasis, in comparison with sufferers at N1 stage. Sufferers who had undergone earlier surgical procedure for major tumor had been at lesser threat of creating mind metastasis as in comparison with sufferers who had not (aOR 0.210, 95% CI 0.131–0.337). Race, histology, liver metastasis, tumor dimension and T stage weren’t important predictors of mind metastasis (Desk 2).
Comparability of diagnostic efficacy of threat components for gastric most cancers mind metastasis
We constructed ROC curves to find out the diagnostic energy of threat components for mind metastasis in gastric most cancers sufferers (Fig. 1). The AUC for various threat components had been in contrast. The outcomes confirmed that the AUC for surgical procedure was 0.704 (95% CI 0.684–0.724, p < 0.001), AUC for web site was 0.557 (95% CI 0.523–0.590, p < 0.001); AUC for histological kind of tumor was 0.515 (95% CI 0.487–0.544, p = 0.305); the AUC for grade was 0.570 (95% CI 0.542–0.598, p < 0.001); the AUC for tumor dimension was 0.638 (95% CI 0.610–0.666, p < 0.001); the AUC for gender was 0.557 (95% CI 0.529–0.586, p < 0.001); the AUC for T stage was 0.675 (95% CI 0.646–0.704, p < 0.001); the AUC for N stage was 0.619 (95% CI 0.590–0.649, p < 0.001); the AUC for age was 0.550 (95% CI 0.520–0.580, p = 0.001); the AUC for bone metastasis was 0.640 (95% CI 0.607–0.674, p < 0.001); the AUC for liver metastasis was 0.626 (95% CI 0.594–0.658, p < 0.001); the AUC for lung metastasis was 0.654 (95% CI 0.620–0.687, p < 0.001); the AUC for race was 0.550 (95% CI 0.522–0.578, p = 0.001); the AUC for revenue was 0.505 (95% CI 0.477–0.534, p = 0.721). Surgical procedure of major tumor was one of the best diagnostic predictor for mind metastasis.
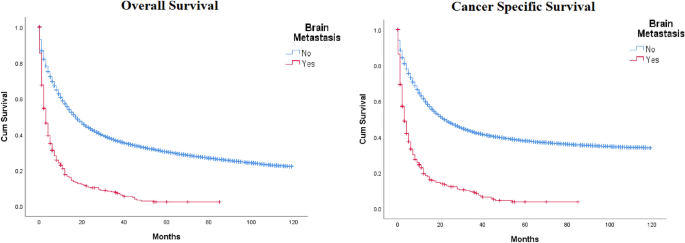
Survival evaluation
The median OS was 3.0 months (95% CI 2.449 ~ 3.551) in sufferers with mind metastasis and 17 months (95% CI 26.778 ~ 33.222) in sufferers with out mind metastasis (p < 0.05) (Fig. 2). The 1, 2, and 4-year OS of sufferers with mind metastasis had been 14.4%, 8.42%, and 1.62%, respectively. The 1, 2 and 4-year OS of sufferers with out mind metastasis had been 49%, 33%, and 17.96%, respectively. The median CSS of sufferers with mind metastasis was 3.0 months (95% CI 2.313 ~ 3.687). For sufferers with out mind metastasis, the median CSS was 22 months (95% CI 21.397 ~ 22.603) (p < 0.05).
Univariable and multivariable evaluation of things affecting the prognosis of sufferers with mind metastasis in gastric most cancers
Univariable Cox regression evaluation of sufferers with mind metastasis confirmed that bone metastasis, no earlier surgical procedure, grade 4 tumor, unknown N stage and first tumor of antrum, physique, higher curvature and overlapping/non-specified web site of major tumor had been important predictors of worse OS (Tables 3, 4).
All important components from the univariable evaluation had been entered into the multivariable Cox regression mannequin. Sufferers who underwent surgical procedure of major tumor had considerably higher OS in comparison with sufferers who didn’t endure surgical procedure (adjusted hazard ratio [aHR] 0.452, 95% CI 0.269–0.758). Grade IV sufferers had a worse OS in comparison with sufferers with Grade I tumors (aHR 5.322, 95% CI 1.114–25.415). Sufferers with major tumors of antrum (aHR 1.957, 95% CI 1.122–3.414) and higher curvature (aHR 2.339, 95% CI 1.238–4.422) had considerably worse OS in comparison with sufferers with major tumor of cardia. Sufferers with unknown N stage had considerably worse OS in comparison with sufferers at N1 stage (aOR 1.372, 95% CI 1.026–1.834) (Desk 3).
Univariable Cox regression evaluation of sufferers with mind metastasis confirmed that bone metastasis, no surgical procedure, grade IV tumor, unknown N stage and first tumor of antrum, physique, higher curvature and overlapping/non-specified web site of major tumor had been important predictors of worse CSS (Desk 3).
All important components from the univariable evaluation had been entered into the multivariable Cox regression mannequin. Sufferers who underwent surgical procedure for major tumor had considerably higher CSS in comparison with sufferers who didn’t endure surgical procedure (aHR 0.458, 95% CI 0.268–0.781). Grade IV sufferers had a worse CSS in comparison with sufferers with Grade I tumors (aHR 5.287, 95% CI 1.106–25.268). Sufferers with major tumors of antrum (aHR 1.858, 95% CI 1.045–3.302) had considerably worse CSS in comparison with sufferers with major tumor of cardia. Sufferers with unknown N stage had considerably worse CSS in comparison with sufferers at N1 stage (aOR 1.390, 95% CI 1.027–1.881) (Desk 3).