Affected person traits
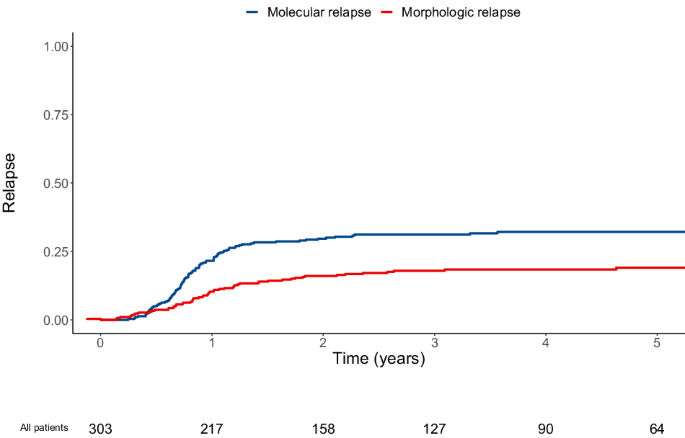
Between 01/01/2010 and 12/31/2019, 303 sufferers from 9 facilities with newly identified CBF or NPM1-mutated AML (RUNX1::RUNX1T1, 19%; CBFB::MYH11, 27%; NPM1, 53%) who have been in first full remission and who had MRD monitoring after first-line intensive chemotherapy have been included. Within the 266 sufferers evaluated for FLT3 mutational standing, 40 had a FLT3-ITD mutation (all however two with concomitant NPM1 mutation) and two had a FLT3-TKD mutation (one with concomitant NPM1 mutation). Amongst included sufferers, 153 (51%) by no means relapsed (median follow-up of 1648 days after first CR; interquartile vary [IQR]: 1101–1976), 95 (31%) had molecular relapse, with a median of 288 days (IQR: 229–384) from first CR, and 55 (18%) had upfront morphologic relapse (i.e., with out prior molecular relapse detected), with a median of 351 days (IQR: 240–519; Fig. 1; Fig. 2). Among the many 95 sufferers with molecular relapse, 53 (56%) obtained preemptive remedy (“preemptive” group with a median of 49 days [IQR: 27–75] from molecular relapse to remedy initiation) whereas 42 (44%) progressed to morphologic relapse by the point salvage remedy was initiated (“mol-morphologic relapse” group with a median of 62 days [IQR:38–132] from molecular relapse to remedy initiation at which level morphologic relapse was noticed; Fig. 1). Though the cumulative incidence of morphologic relapse at three years was comparable between sufferers with RUNX1::RUNX1T1, CBFB::MYH11, and NPM1-mutated AML (18% [8–28%], 16% [8–24%], and 19% [13–25%], respectively), the cumulative incidence of molecular relapse was decrease in sufferers with RUNX1::RUNX1T1 AML (23% [12–34%], 31% [21–41%], and 34% [27–42%], respectively); Supplementary Fig. 1). Molecular relapse occurred later in sufferers with RUNX1::RUNX1T1 AML (median of 377 days [269–452] vs. 269 [199–371] vs. 279 [233–371]) whereas morphologic relapse occurred earlier in these sufferers (median of 288 [170–570] vs. 337 [305–456] vs. 355 [245–527]). There was a big correlation between BM and PB MRD in sufferers for whom paired outcomes have been out there, both after post-induction (n = 93; P < 0.001), at greatest response throughout first-line remedy (n = 161; P < 0.001), or at molecular relapse (n = 34; P < 0.001; Supplementary Fig. 2). With a quantification cut-off of 0.001%, 94 samples at greatest response have been concordant whereas 64 samples have been evaluated as adverse in PB however constructive in BM and three as constructive in PB and adverse in BM. Among the many 34 paired samples out there at molecular relapse, three have been solely detectable in BM whereas all others have been detectable in PB and BM.
Sufferers with molecular and upfront morphologic relapse had larger white blood cell (WBC) rely at analysis (12 vs. 22 vs. 30 G/l in these with out relapse, molecular relapse, and morphological relapse, respectively, P = 0.003) and had decrease MRD log-reduction in PB after induction remedy (4.15 vs. 3.71 vs. 3.64, respectively, P = 0.04). Greatest MRD response throughout first-line remedy was not totally different between the three teams. As well as, sufferers with upfront morphologic relapse have been extra more likely to have CR with constructive MRD apart from CRMRD-LL by the tip of remedy in peripheral blood (2% vs. 16% vs. 32%, respectively, P < 0.001) and to have obtained lower than three consolidation cycles (7% vs. 7% vs. 22%, respectively, P = 0.003; Desk 1). Sufferers with any degree of MRD within the bone marrow after first-line remedy have been extra more likely to have molecular relapse whereas virtually all sufferers with MRD apart from CRMRD-LL in peripheral blood (n = 22) finally relapsed, both molecularly or morphologically (Supplementary Fig. 3). Related outcomes have been noticed when sufferers with CBF and NPM1-mutated AML have been analyzed individually or when sufferers with 2022 ELN favorable AML (i.e., CBF and AML with NPM1 mutations and with out FLT3-ITD mutations) have been thought-about (Supplementary Tables 1 to 3). Nonetheless, extra sufferers with NPM1 and FLT3-ITD mutations skilled molecular and morphologic relapse (12% vs. 34% vs. 29%, respectively, P = 0.01, Supplementary Desk 2). There was no distinction in affected person traits in response to the kind of relapse (“preemptive”, “mol-morphologic relapse”, and “upfront morphologic relapse” teams) in addition to much less consolidation cycles obtained throughout first-line remedy in sufferers with upfront morphologic relapse (Supplementary Desk 4).
End result of sufferers in response to the kind of relapse
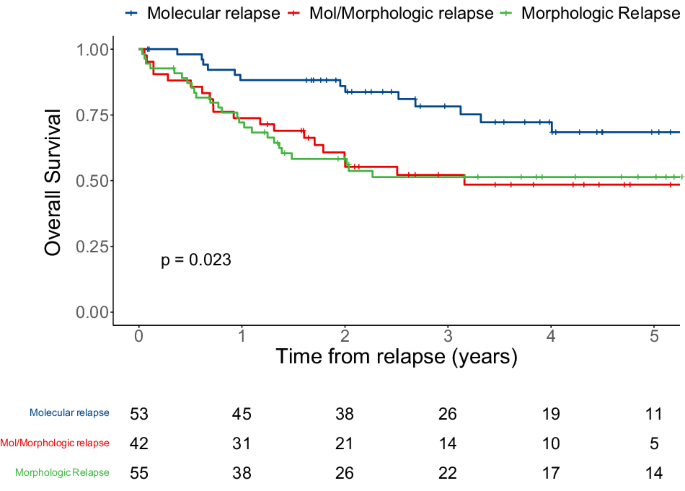
The multistate mannequin and the variety of sufferers getting into the state transition matrix are described in Fig. 1A. Throughout follow-up of the entire cohort, 50% of sufferers stayed alive and in remission (with solely 3 deaths in sufferers who remained in remission). In sufferers who relapsed, predicted chances of being alive after preemptive remedy for molecular relapse or after morphologic relapse have been 13 and 17%, respectively, whereas 4% died after preemptive remedy for molecular relapse and 15% after morphologic relapse (Fig. 1B). Sufferers who obtained preemptive remedy had a greater OS than those that obtained salvage remedy after having progressed from molecular to morphologic relapse, and those that had upfront morphologic relapse (three-year OS of 78% vs. 52% vs. 51%, respectively, P = 0.02; Fig. 3), as when contemplating CBF and NPM1-mutated AML affected person individually (Supplementary Fig. 4). Related outcomes have been noticed when calculating survival chances from the day of beginning salvage remedy after excluding two sufferers who declined salvage remedy, relatively than on the day of first detected relapse (Supplementary Fig. 5). Curiously, treatment-related mortality was considerably larger in sufferers who obtained salvage remedy whereas in morphologic relapse (P = 0.015; Supplementary Fig. 6).
General survival of 150 sufferers with CBF or NPM1-mutated AML who relapsed throughout follow-up, stratified by the kind of relapse (molecular relapse with preemptive remedy vs. molecular relapse with morphologic relapse on the time of salvage remedy vs. upfront morphologic relapse), calculated from the time of first detected relapse.
To review the connection between the kind of relapse and outcomes in additional element, we evaluated univariable and multivariable regression fashions for the endpoint of OS calculated from the time of first detected relapse. In univariable evaluation, age at analysis (hazard ratio [HR] = 1.03 [1.01–1.06], P = 0.022), variety of consolidation cycles (HR = 0.59 [0.35–0.99], P = 0.046), greatest MRD log discount in bone marrow (HR = 0.66 [0.51–0.85], P = 0.001), CR with MRD apart from at low-level in bone marrow and in peripheral blood on the finish of first-line remedy (HR = 2.20 [1.08–4.50], P = 0.03, and HR = 2.25 [1.07–4.73], P = 0.033, respectively), and each “mol-morphologic” and upfront morphologic relapses (HR = 2.34 [1.16–4.71], P = 0.017, and HR = 2.31 [1.18–4.51], P = 0.015) have been related to OS (Desk 2). After multivariable adjustment, excluding potential colinear variables, greatest MRD log discount in bone marrow (HR = 0.71 [0.55–0.93], P = 0.011) and “mol-morphologic” relapse (HR = 2.17 [1.00–4.71], P = 0.05) have been independently related to OS.
Salvage remedy
The kind of salvage remedy for the “preemptive”, “mol-morphologic relapse”, and “upfront morphologic relapse” teams are described in Desk 3. Time from relapse detection to salvage remedy initiation was considerably shorter in sufferers with upfront morphologic relapse (P < 0.001). Though not statistically totally different, sufferers with molecular relapse who obtained preemptive remedy whereas in molecular relapse had a shorter time to remedy than sufferers who’ve progressed to morphologic relapse at remedy initiation (49 vs. 62 days; P = 0.08). Additionally, considerably extra sufferers within the “preemptive” group obtained upfront allogeneic HCT (19 [36%] vs. 2 [5%] vs. 2 [4%] within the “preemptive”, “mol-morphologic relapse”, and “upfront morphologic relapse” teams, respectively).
Salvage remedy with intensive chemotherapy was additionally much less frequent within the “preemptive” group (21 [40%] vs. 33 [79%] vs. 41 [75%], respectively; P < 0.001). Among the many 19 sufferers within the “preemptive” group receiving upfront allogeneic HCT, 11 of them obtained transplant from a HLA-matched sibling donor and 6 obtained a sequential conditioning routine. The speed of allogeneic HCT was comparable between the three teams (85% vs. 74% vs. 82%, P = 0.38). Among the many 28 sufferers who didn’t endure transplant (19%), solely 7 have been nonetheless alive at three years (RUNX1::RUNX1T1 [n = 1], CBFB::MYH11 [n = 4], and NPM1 mutation [n = 2]; molecular relapse [n = 6], morphologic relapse [n = 1]; Supplementary Fig. 7).
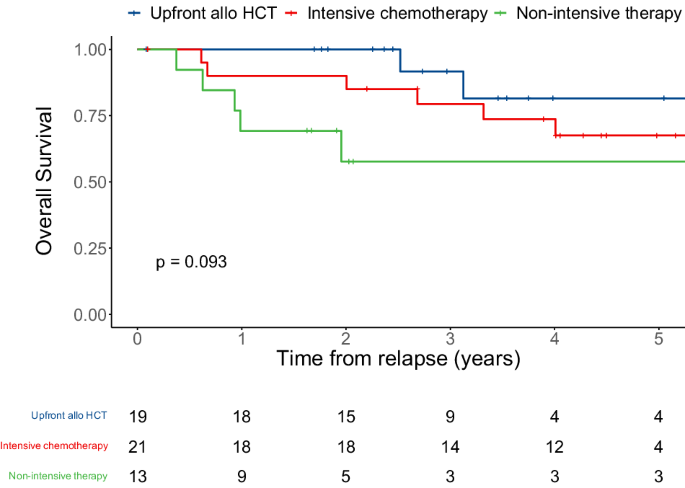
Particular outcomes of every class of preemptive remedy (upfront allogeneic HCT [n = 19], intensive chemotherapy [n = 21], and non-intensive remedy [n = 13]) are summarized in Supplementary Desk 5. Within the 19 sufferers who proceeded to upfront allogeneic HCT, 15 (79%) achieved full molecular remission after allogeneic HCT with solely two relapsing after allogeneic HCT. Extra sufferers achieved full molecular remission after intensive chemotherapy compared to sufferers who obtained non-intensive chemotherapies (11 [52%] vs. 2 [15%]) and had decrease ranges of transcript earlier than allogeneic HCT (0.003 [0.001–0.29] vs. 2.5 [0.01–11.3]). Completely different OS charges, that didn’t attain statistical significance, have been noticed between the three remedy methods (92% vs. 79% vs. 58% at three years for upfront allogeneic HCT, intensive chemotherapy, and fewer intensive remedy, respectively, P = 0.09; Fig. 4). Two-by-two comparisons confirmed that there was a big distinction in OS between sufferers receiving upfront allogeneic HCT and non-intensive chemotherapy (P = 0.027) whereas OS of sufferers receiving upfront allogeneic HCT and intensive chemotherapy (P = 0.36) and OS of sufferers receiving intensive and non-intensive chemotherapy weren’t totally different (P = 0.24).
General survival of 53 sufferers with CBF or NPM1-mutated AML with molecular relapse who obtained preemptive remedy, stratified by the kind of salvage remedy (upfront allogeneic hematopoietic cell transplantation (HCT) vs. intensive chemotherapy vs. non-intensive chemotherapy), calculated from the time of first detected relapse.