The Unfavorable Mammogram: A digital mammogram of the precise and left breast of a 51-year-old affected person with dense breast tissue from February 15, 2023. Nothing seems irregular.
Picture: Courtesy of Dr. Christiane Kuhl
In the midst of the night time, Angie McCoy flipped onto her abdomen in mattress and felt one thing exhausting in her proper breast. It was July 2020, and she or he and her husband, Tim, had been staying at a rental home in Texas Hill Nation whereas they waited for the development of their new residence to be completed. She didn’t know find out how to describe the feeling — it wasn’t fairly a lump, however one thing about it felt off. It was most pronounced when she lay in opposition to a agency floor.
The following day, McCoy made an appointment with a normal practitioner, who referred her for a mammogram and an ultrasound. The radiologist instructed her that each of these scans had been destructive — he couldn’t see something that indicated most cancers. “I feel we’re simply coping with dense breast tissue,” he stated, including that she ought to come again in six months for retesting simply to make certain. Dense breast tissue. This was nothing new: Radiologists had at all times talked about that McCoy had dense breasts, however she didn’t perceive what it meant or why she ought to care. None of her medical doctors had ever stated this is likely to be trigger for concern.
Six months later, in February, she had one other mammogram and ultrasound. The medical doctors, once more, stated that each had been destructive. However the hardness in her breast was nonetheless there. McCoy ran via attainable explanations in her head: At 52, she was perimenopausal, so her breasts would typically harm and had been generally swollen. In addition to, she trusted medical doctors — her personal late father was a radiologist.
By the summer time of 2021, the hardness had begun to really feel like a ridge on the backside of her breast. In the future in July, McCoy was studying a guide on her entrance porch when an excruciating ache started to radiate from her proper armpit down previous her elbow. That night time in mattress, she was awoken by a sudden ache not like something she’d skilled earlier than. She seemed down and noticed that her proper breast was severely infected. McCoy stood up, walked over to her rest room mirror, and lifted her pajamas. What she noticed astounded her: That breast was cartoonishly giant, practically double the dimensions of the left. It was so outstanding that “for the primary time ever in my life, and possibly the final,” she took a photograph of herself bare. Days later, she confirmed the picture to her primary-care supplier. The physician dismissed it as nothing severe however ordered one more mammogram and ultrasound.
Two weeks later, McCoy was again on the radiologist’s workplace. “Excellent news!” he declared. “Each scans are destructive.” He requested her to indicate him what was bothering her. “Can you are feeling this deep ridge?” she requested. “Do you see how infected the precise breast is?” Sure, he may really feel it, however he may see nothing regarding on the mammogram. He instructed her that if she needed to be completely sure, she may get a biopsy. Additionally, he stated, if something adjustments, she may schedule one other appointment.
McCoy walked out into the car parking zone and stood there in anger. If something adjustments? She was an obedient individual and had at all times listened to medical doctors, but it surely had been a yr since she first felt that odd hardness in her proper breast. To her, all the adjustments that had taken place in her physique since then signaled one thing distinct and alarming. Later that day, she known as her primary-care physician and requested to see a specialist. She acquired an appointment for six weeks later with a breast surgeon who she was instructed may order extra assessments.
The summer time dragged on. Her breasts grew more and more sore, aching every day. Throughout Pilates class, she’d be mendacity face down on a field atop the reformer machine and really feel the mass, agency as an unripe avocado. When she lastly had her biopsy in early September, the pores and skin of her proper breast was so taut that the nipple was retracted. The biopsy was adopted by an MRI. McCoy was strolling the three-mile loop in her neighborhood the following day when she acquired the decision from the surgeon: metastatic breast most cancers. “It seems like there are a number of extremely suspicious metastatic lesions in your sternum, ribs, and clavicle,” the surgeon stated. It was a scorching, dry afternoon. She hung up and stared down at her cellphone.
Two weeks later, McCoy acquired her first PET scan, a delicate imaging check that medical doctors use to find out how far most cancers has unfold in organs and tissues. It confirmed that McCoy had most cancers in all of her bones. “Nostril to knees,” she was instructed. “Innumerable lesions.” The PET scan resembled one among Jackson Pollock’s canvases, like somebody had splattered paint throughout her skeleton. It had metastasized up to now that the sorts of therapy obtainable for earlier-stage breast most cancers — a lumpectomy, a mastectomy — had been now not an possibility.
McCoy thought again on her years of compliance with medical doctors, on her close to decade of yearly mammograms with by no means an irregular end result. “I had executed every part proper. I’ve executed every part I used to be imagined to do,” she says. “It was devastating realizing that the most cancers was rising all the time.”
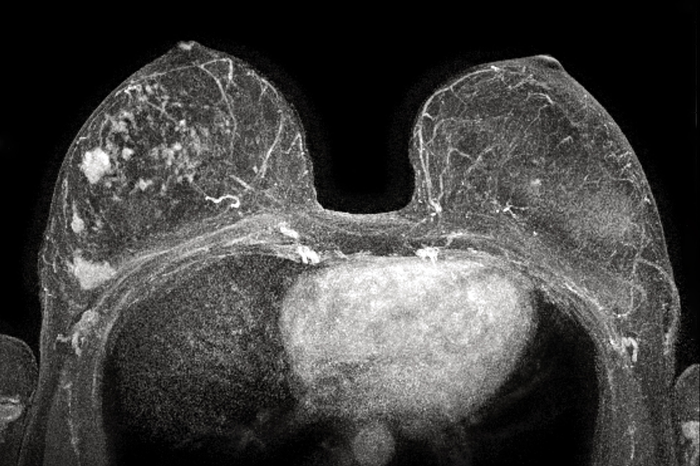
The Constructive MRI: An MRI of the identical affected person three months after her mammogram. The MRI depicts as many as three cancers in her proper breast plus some precancerous lesions, all of which had been invisible on her mammogram.
Picture: Courtesy of Dr. Christiane Kuhl
Get your mammogram! is a directive that each one American ladies hear from an early age. That is due, partly, to probably the most efficient public-health campaigns in medical historical past. The primary cases of mammography produced pictures of unreliable or various high quality, however within the late Fifties, a Houston radiologist named Robert Egan standardized a brand new approach that not solely yielded clear, reproducible scans but additionally dependably picked up cancers that bodily exams had missed or that appeared in ladies with no signs. Within the mid-Sixties, utilizing Egan’s technique, a group of radiologists in a van outfitted with X-ray machines parked beside ice-cream vehicles in midtown Manhattan and screened 62,000 ladies on their lunch breaks.
Over the following 4 many years, mammograms would turn out to be the gold normal for breast-cancer detection. Within the early Eighties, the American Most cancers Society started recommending mammograms each one to 2 years for girls over the age of 40, a advice it could replace to yearly in 1997. Expanded media protection, screening applications, and campaigns like the worldwide “Flip your metropolis pink!” initiative — typically sponsored by mammography-makers like Siemens — inspired ladies over the age of 40 to hunt common mammograms for early detection of breast most cancers. At this time, yearly mammograms are coated by most main health-insurance plans, in addition to by Medicaid, for girls 40 and older. Walmart has even begun rolling out a pilot program by which folks can get their yearly mammogram in-store.
Mammograms have decreased the mortality from breast most cancers by 40 p.c since 1990. However in early research of Egan’s approach, multiple in 5 ladies acquired a false-negative end result by which mammograms didn’t detect most cancers completely. And even because the expertise superior — as corporations like DuPont launched screen-film and digital mammography, which make the imaging course of each sooner and better distinction, and 3-D mammograms that take pictures from a number of angles — the issue of missed cancers has remained.
Because the aughts, specialists within the breast-imaging and breast-surgery world have recognized one issue that may make it tougher for a mammogram to detect most cancers: breast density. The breast is made up of three sorts of tissue: glandular tissue, which incorporates the lobules that produce milk; fibrous connective tissue, which incorporates the ducts that ship the milk to the nipples; and fatty tissue, which fills the area in between. When a breast incorporates extra glandular and connective tissue than fatty, it’s labeled as dense.
On a mammogram, fatty tissue seems as darkish grey or black. Most cancers tissue, which exhibits up as white, ought to stand out in stark reduction. However dense breast tissue additionally exhibits up as white and might fully obscure a malignant white mass. Elisa Port, the chief of breast surgical procedure for the Mount Sinai Well being System in New York, has in contrast discovering most cancers in a dense breast on a mammogram to recognizing a polar bear in a snowstorm. “White on white is troublesome to see in opposition to the background,” she says. In a fatty breast, mammograms are as much as 98 p.c correct; in an especially dense breast, the accuracy may be as little as 30 p.c. Generally a lady with dense breasts would possibly complement her mammogram with an ultrasound. “That’s a straightforward check to do, however everybody has this false impression that an ultrasound goes to shut the hole completely,” Port says. “An ultrasound will solely choose up about one or 2 p.c additional of cancers.” That is hardly a fringe downside. Half of ladies within the U.S. have dense breasts, and, difficulties of detection apart, ladies with dense breast tissue are additionally at larger danger for creating most cancers, although clinicians aren’t positive why.
“We all know what the most effective screening technique can be, however we fail to make use of it,” says Christiane Kuhl, who serves as chair of radiology at RWTH Aachen College Hospital in Germany. In line with Kuhl, it has been uncontroversial amongst radiologists and different specialists for many years that essentially the most delicate instrument for early detection of breast most cancers is the MRI. Throughout a breast MRI, a affected person lies face down with arms both overhead or by their sides and enters the MRI machine, which makes use of a big magnet, radio waves, and a pc to supply sharp, detailed pictures of far larger distinction decision than mammograms. Again in 2007, Kuhl printed a examine in The Lancet that examined the outcomes of most cancers screens for greater than 7,000 ladies and located that mammograms missed 48 p.c of ductal carcinoma in situ (the earliest type of breast most cancers), whereas MRIs missed 2 p.c. And in dense tissue, tumors and much will present up on a breast MRI as distinctly white in opposition to a black background.
Organizations like DENSE (Density Training Nationwide Survivors’ Effort) have been making an attempt over the previous decade to boost consciousness about breast density and the extra downside it poses in mammograms, and as of final yr, 38 states had enacted legal guidelines that require medical facilities to ship letters to ladies informing them if they’ve dense breasts. (In 2023, the FDA made this observe a nationwide coverage, and the remaining 12 states have till September 2024 to implement it.) Nonetheless, even when ladies are notified, hardly ever are they warned about its implications or given directions to pursue additional testing. Hospitals, primary-care medical doctors, and OB/GYNs haven’t modified their protocols when screening ladies with dense breasts. Often, the burden rests on the affected person.
When she was 34, Katy Weade, a life and well being coach in Illinois, started getting common mammograms after discovering a benign cyst in her breast. However Weade has dense breast tissue, and it was solely upon getting an MRI at age 41 that she realized she had stage-three breast most cancers. It had unfold to her lymph nodes. She posted a video concerning the expertise on Instagram, and someday she acquired a DM from a stranger who had seen her put up. Regardless of years of fresh mammograms, the girl had just lately discovered a rocky lump in her breast and was impressed by Weade to request further screening. “I’m praying for you that it seems to be nothing. Please maintain me posted!” Weade wrote again.
“Thanks, I simply left a message for my physician with the nurse’s station,” the girl replied. Two weeks later, she despatched Weade {a photograph} of a chunk of paper. It was the outcomes of her further assessments, and on it was written “Invasive carcinoma with mucinous options. Giant tumor however nonetheless thought of Grade 1.”
Many sufferers need to exhibit excessive tenacity so as to persuade their medical doctors to order supplemental testing. In August 2022, Tina Paxton, a instructor in Texas, skilled ache so extreme in her proper breast that it could “ship me to my knees.” Her physician was satisfied she had solely pulled a muscle working, and for months he instructed her to up her dosage of Excedrin.
By November, Paxton was again in his workplace. The ache hadn’t gone away. He instructed her it was in all probability simply the stress of the approaching vacation season. It wasn’t implausible: “I used to be what you’ll contemplate a go-getter,” she tells me. “I’ve three boys. I used to be loopy about Christmas and the vacations. I volunteered for every part.” The physician additionally reminded her that she’d had a clear mammogram of her dense breast tissue simply seven months earlier.
“You once more?” he requested when she returned to his workplace for the third time after the vacations. “If it could appease you, I’ll order an ultrasound,” he stated. When she went in for the examination in January 2023, she may hear the medical doctors arguing outdoors her room. Then they instructed her they might carry out a biopsy, too. The outcomes started to come back within the subsequent day: The prognosis was triple-negative, a difficult-to-treat type of most cancers with a better mortality charge. When Paxton lastly met with an oncologist every week later, the physician may really feel the tumor instantly.
One cause medical doctors hardly ever order supplemental screens like MRIs is value: MRIs are ten occasions costlier than mammograms, and insurance coverage corporations virtually by no means cowl them. Below most plans, dense breasts alone don’t qualify ladies for MRIs with out being coupled with different danger components resembling household historical past and genetic markers. And if these supplemental screens aren’t coated, they will value greater than $1,000 out of pocket, which deters many ladies from getting them. MRI machines are additionally more durable to seek out, particularly in rural areas, and lots of health-care amenities and breast-screening facilities don’t have them.
In the meantime, mammograms stay such a staple requirement that I’ve encountered ladies who stated that, even after their breast most cancers was confirmed by a biopsy or an ultrasound, their insurance coverage corporations refused to pay for an MRI till they acquired a mammogram. As soon as, one among Kuhl’s sufferers had an MRI that detected breast most cancers, however even with the constructive end result, her insurance coverage denied protection of the examination, demanding that she obtain a mammogram. So Kuhl ordered one. It got here again clear.
Even when medical doctors know that mammograms have missed breast most cancers in a affected person with dense breast tissue, they generally nonetheless depend on mammograms to display for whether or not the most cancers will return. Shamara Jackson Knowlton was in highschool when her mom, Pamela, first felt a lump in her breast. Like many ladies, Pamela was at all times instructed she had dense breast tissue, however not one of the medical doctors at her small-town clinic in Virginia had ever defined the importance of it. (Black ladies like Pamela are additionally extra prone to have dense breast tissue.) After years of destructive mammograms, Pamela was identified with stage-three breast most cancers in 2010 via her first MRI. She underwent chemo and radiation, and medical doctors continued to order mammograms to see whether or not the most cancers had shrunk.
For years following Pamela’s remedies, Shamara believed her mom was doing properly. They spoke every day on Shamara ’s drives to and from work, and her mom hardly ever talked about most cancers and appeared to be feeling higher. In April 2012, Pamela acquired one other mammogram and was instructed she had a clear invoice of well being, Shamara remembers. The medical doctors instructed her she was in remission.
Two months later, Pamela’s well being started to deteriorate. It began with nasal congestion, which she believed was a sinus an infection. Then in July, she handed out at work, and a CT scan and MRI of her mind didn’t yield clues why. By the tip of the month, a golf-ball-size lump had appeared on the again of her neck, and she or he started to expertise blurred imaginative and prescient.
Shamara had graduated school, and she or he started to accompany her mom to all of her appointments. She remembers how exhausting she needed to push to get medical doctors to take her mom’s considerations significantly. “I feel the most important factor with my mother and so many ladies isn’t being an advocate as a result of they don’t know what inquiries to ask,” Shamara tells me. “I’d say, ‘My mother has very dense breasts. As a substitute of simply doing a mammogram, why aren’t we doing an MRI? Are we going to do an ultrasound as properly?’ ” After parsing medical research on-line, Shamara began to fret the lump on her mom’s neck may sign the return of most cancers, however medical doctors dominated out the likelihood when a spinal faucet didn’t detect most cancers cells in her spinal fluid.
By mid-August, Pamela had gone blind. One afternoon in September, Shamara was on the playground together with her son when her cellphone rang. It was Pamela. She had simply realized that the lump in her neck was, in reality, most cancers, and that it had metastasized from her breast to the again of her neck and her mind. Pamela was instructed she had six to eight weeks to stay.
For Shamara, the information made for the worst type of vindication. “It was gut-wrenching,” she tells me. “I had been at that hospital for 2 or three weeks. I nonetheless bear in mind the physician sitting on the stool beside my mother’s mattress, and my sister and I standing up, saying, ‘She has to have mind most cancers.’” Shamara helped her mom get right into a cancer-treatment heart in Philadelphia, however by the next yr, it was clear there have been no additional remedies that might assist her. Pamela was positioned on hospice till she died in Could 2013.
Final yr, payments to mandate insurance coverage protection of supplemental screens like MRIs for high-risk ladies had been enacted in 11 states. In Pennsylvania, a regulation went into impact in 2022 that requires insurance coverage corporations to cowl breast MRIs for high-risk ladies. As of early 2024, 20 states have handed laws lowering out-of-pocket prices for supplemental scans medical doctors deem medically needed. Different payments are sitting earlier than Congress, just like the Entry to Breast Most cancers Analysis Act and the Discover It Early Act, which each try to get rid of all out-of-pocket prices for screening, together with MRIs.
Nonetheless, the health-care group is split concerning the cost-effectiveness of offering MRIs for girls with dense breasts. Port, as an example, identified that mammograms are essentially the most cost-effective screening instrument and that total they save many lives. It’s not possible, she believes, to supply an MRI to each lady with dense breasts. “Why don’t 20-year-olds get colonoscopies?” she asks. “Why don’t we do screening CT scans for lung most cancers in each single individual?” There are dangers with each process, even these usually thought of protected, and additional testing may result in extra alternative for hurt: A false constructive on an MRI scan may result in an unneeded biopsy, for instance. Port believes MRIs needs to be reserved for girls with each dense breasts and another type of elevated danger, resembling household historical past.
In a single influential 2009 paper, researchers developed a predictive mannequin that concluded that, whereas MRIs could also be extra delicate than mammograms for high-risk ladies, the extra variety of quality-adjusted years that routine breast MRIs may add to their lives was not a lot larger than the quantity added by routine mammograms. In the meantime, the mannequin discovered that MRIs would value $18,200 over 25 years, whereas mammograms would value solely $4,800. (The examine was partially funded by the PhRMA Basis, a nonprofit that receives donations from pharmaceutical corporations that make most of the world’s top-selling most cancers medication.)
In April 2024, a nationwide panel of well being specialists at the USA Preventive Companies Activity Drive issued its newest suggestions for breast-cancer screening. The duty power is enormously influential, largely dictating what most personal and government-funded insurance coverage corporations will cowl. This yr, it concluded that, even for girls with dense breasts, there wasn’t adequate proof to evaluate “the stability of advantages and harms of supplemental screening” like ultrasounds or MRIs. In its suggestions, the duty power cited a lot of research. One in every of them, primarily based on historic insurance coverage claims, urged that MRIs usually tend to result in “cascade occasions” — visits to the physician’s workplace, hospitalizations, and new diagnoses. Because the USPSTF’s record of beneficial preventative providers gained’t embrace further screening instruments like MRIs primarily based on breast density alone, insurance coverage corporations is not going to need to cowl them.
Some advocates are suspicious of this line of logic about the price of MRIs. “The way in which federal payments are scored, they don’t have a look at the long run financial savings. We all know that if you will get folks into this imaging, you’re doubtless going to catch their illness earlier,” says Molly Guthrie, vice-president of coverage and advocacy at Susan G. Komen. “It’s additionally going to be cheaper for the health-care system and for the insurers,” she continues, “since you’re going to be treating somebody with early-stage breast most cancers in comparison with stage 4, after they’ll be in therapy for the remainder of their life.”
Guthrie hopes it’s solely a matter of time earlier than insurance coverage insurance policies meet up with the present analysis. “It wasn’t that way back that individuals needed to pay out of pocket for his or her yearly mammograms,” she says. Insurance coverage corporations had been solely required to start protecting them after the Reasonably priced Care Act included such preventative providers via the USPSTF in 2010. In the meantime, radiologists like Kuhl are optimistic about an alternate type of the check known as abbreviated MRIs. They happen in the identical machine, however the process is accomplished in beneath ten minutes at a fraction of the price.
On the September day that Angie McCoy realized she had superior breast most cancers, she dialed her husband’s quantity and matter-of-factly reported what the physician had instructed her. However when she known as her greatest buddy, her composure dissolved. It took saying the knowledge aloud a second time for it to start out sinking in. “I actually couldn’t get the phrases out of my mouth,” she remembers. “I couldn’t really feel my lungs. It’s like my physique was convulsing in worry.” Stage-four breast most cancers: “I’d executed sufficient studying to know what that meant,” she says. “That meant that I might have a shortened lifespan and that I might be in therapy for the remainder of my life.”
From October 2021 till February 2022, McCoy had six rounds of four-hour-long chemo infusions that introduced near-constant bouts of nausea, diarrhea, and fatigue. Even when chemo and radiation assist management it, a prognosis of stage-four breast most cancers can imply a lifetime of most cancers therapies. At this time, McCoy takes a handful of tablets every day and will get common infusions of Herceptin and Perjeta, two medication that focus on her particular type of most cancers, via a everlasting chest port. The medication value hundreds of {dollars} per dosage, although McCoy has good insurance coverage that covers the drugs after they hit the deductible. She sees an oncologist each different month and will get an echocardiogram each three months and a PET scan each six.
Whereas she was present process chemo, her son Jacob was ending his remaining semester at Oklahoma Metropolis College with a level in music composition. His senior capstone challenge was an orchestral efficiency of his personal authentic composition. McCoy’s immune system was battered from the remedies, and a COVID variant was surging, so her son’s professor organized for her household to look at the efficiency from an commentary room away from the remainder of the viewers.
Each Jacob and his elder brother are of their 20s; McCoy had them younger sufficient that she had at all times assumed she can be there for the massive moments of their lives: school graduations, marriages, grandchildren. Now, all of that felt unsure. “You’re messing with folks’s lives once you don’t go the additional yard and ship us for a breast MRI,” McCoy says. “Girls like me are paying for it in misplaced time. It’s a little bit black cloud over your head on a regular basis: What number of extra years do I’ve?”